
Scars are a natural part of the body’s healing process after surgery. While they signify the mending of tissues, they can sometimes be a source of concern for patients due to their appearance and potential complications. However, with proper care and attention, scars can heal well and become less noticeable over time. In this blog, we will discuss comprehensive guidelines for scar management after various surgical procedures (labiaplasty, gynecomastia, prominent ear correction, liposuction, facelift, blepharoplasty, breast reduction, augmentation, mastopexy, and lower body lift etc.).
Understanding Surgical Scars
When your skin undergoes trauma, such as during surgery, scarring is a natural part of the healing process. Here is a breakdown of how it happens:
Hemostasis: Initially, blood platelets rush to the incision site to form a scab, preventing blood loss.
Inflammatory Response: Next, white blood cells arrive to fight off infection, leading to redness, swelling, and warmth around the incision.
Cell Proliferation: New cells are created, and collagen, a protein crucial for skin elasticity, is produced. The balance of collagen during this phase influences the scar’s appearance.
Maturation: Over time, the scar tissue matures, gradually fading from reddish to pink or flesh-coloured. However, the final colour may vary depending on your skin type. Scars typically go through different stages of maturation over a period of 18 months to 2 years.
Different types of Scars
Keloid Scars
Keloid scars are thick, raised, and firm scars that extend beyond the boundaries of the original wound or injury. They often appear red or darker than the surrounding skin due to excessive collagen production during the healing process. Keloids can occur anywhere on the body but are more common on the chest, back, shoulders, and earlobes. They tend to develop in darker-skinned individuals and may appear up to a year after the initial trauma.
Hypertrophic Scars
Similar to keloid scars, hypertrophic scars are thick and raised, but their growth is confined within the boundaries of the original wound or incision. Initially red, they eventually become skin-coloured. While hypertrophic scars may improve over time, they typically do not completely flatten out. Early interventions such as pressure, massage and silicone gel/sheeting can help reduce their appearance.
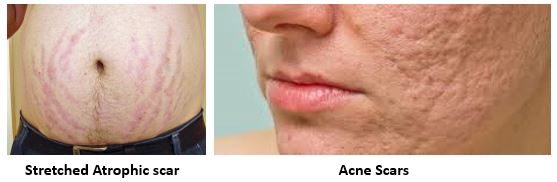
Atrophic Scars
Atrophic scars are characterized by sunken, indented areas in the skin, resembling exaggerated stretch marks. They can result from trauma, surgery, or conditions like severe acne or chickenpox. Unlike keloid and hypertrophic scars, the size and shape of atrophic scars typically remain unchanged over time.
Acne Scars
Scarring related to acne can manifest in three primary forms:
- Ice Pick Scars: Small, narrow, and deep scars that create a pitted appearance on the skin.
- Boxcar Scars: Wider and shallower than ice pick scars, with clearly defined borders.
- Rolling Scars: Shallow and wide scars that lack distinct edges.


How to manage the scars after surgical procedure at MACS Clinic
- Moisturization: Keeping the scar area moisturized is crucial for optimal healing. Moisturizers help to maintain the skin’s hydration, preventing it from becoming dry and reducing the risk of complications such as itching and irritation. Look for gentle, fragrance-free moisturizers and apply them regularly to the scar area.
- Massage: Massaging the scar tissue can help break down scar adhesions and improve circulation, promoting better healing and reducing scar stiffness. Use gentle circular motions with your fingers or a soft massage tool to massage the scar for several minutes each day. This can be started once the wound has fully healed and sutures have been removed, typically after a few weeks.
- Silicone Application: Silicone gel, spray, cream or sheets are widely recommended by healthcare professionals for scar management. Silicone creates a protective barrier over the scar, locking in moisture and promoting an optimal environment for healing. Thinly apply silicone to the scar area once it has fully closed and continue using it for several months to enhance scar maturation.
4. Desensitization: Scars often have reduced sensation due to a limited number of nerve endings. Desensitization techniques can help train the scar tissue to become less sensitive, reducing pain, tenderness, and sensitivity over time. Products like Bio-Oil, Nivea cream, and E45 can be beneficial for desensitizing the scar area.

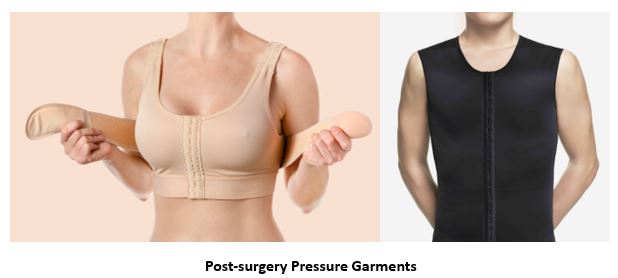
5.Pressure therapy: Pressure garments for scar treatment are specially designed garments worn to reduce hypertrophy within scars. While commonly used for burn scars, they can also be effective for most hypertrophic scars. These garments provide compression therapy to areas of raised scarring, helping to flatten scars and reduce redness by minimizing excess blood supply. By applying constant pressure, pressure garments support the natural scar maturation process. Made of tight-fitting lycra customized to your measurements, they offer several benefits:
- Minimizing scar development by interfering with collagen production
- Protecting fragile skin
- Promoting better tissue circulation
- Reducing pain and itching, and even increasing skin length by applying pressure on contracture bands.
What Happens to the Scar?
Over time, scars undergo a process of maturation, during which they become softer, more supple, and less noticeable. However, complications such as hypertrophic scars, keloids, hyperpigmentation, depigmentation, and scar stretching can occur in some cases. Monitoring the scar’s progress and seeking medical attention if any complications arise are essential for optimal healing.
In conclusion, scar management after surgery involves a combination of general guidelines and specific considerations based on the type of procedure performed. By following these recommendations and maintaining regular follow-ups with Mr. Shailesh Vadodaria, you can promote optimal scar healing and minimize potential complications. Patience and consistency are key when it comes to scar management.


