
Warts (Verruca): Causes, Types, and Treatment Options
A wart (also known medically as verruca) is a small, usually benign growth on the skin or mucous membrane caused by an overgrowth of cells in the upper layer of the skin. While most warts are non-cancerous and self-limiting, some may persist, spread, or resemble more serious conditions such as skin cancers — hence, accurate diagnosis and careful management are essential.
At MACS Clinic, we offer comprehensive diagnostic evaluation and both surgical and non-surgical treatment options for warts, prioritising safety, efficacy, and histopathological confirmation where appropriate.
Causes of Warts
They commonly appear on the:
- Clinical examination by a trained clinician is often sufficient.
- Dermatoscopic evaluation may help differentiate benign from malignant lesions.
- Histopathological examination (biopsy or excision specimen) is the gold standard to confirm diagnosis, rule out malignancy, and identify the exact wart subtype.
Treatment Options
Non-Surgical / Destructive Treatments
- Cryotherapy (liquid nitrogen freezing)
→ Freezes wart tissue, causing it to slough off.
Advantages: Quick, minimal downtime.
Disadvantages: Painful; may require multiple sessions; no tissue for histopathology. - Chemical Cauterisation
→ Application of salicylic acid or trichloroacetic acid to destroy infected tissue.
Advantages: Simple and inexpensive.
Disadvantages: Needs regular application; risk of skin irritation; no diagnostic sample. - Electrocoagulation / Radiofrequency Ablation / Laser Therapy
→ Energy-based destruction of wart tissue.
Advantages: Rapid clearance.
Disadvantages: No tissue available for histology; small risk of scarring and recurrence.
They are not contagious and not related to skin cancer, although they can sometimes resemble one.
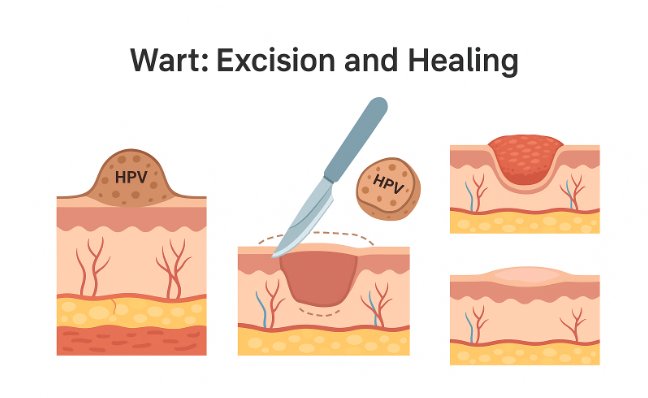
Surgical Excision (Preferred at MACS Clinic)
At MACS Clinic, we frequently recommend minor surgical excision under local anaesthesia for diagnostic and therapeutic purposes.
Advantages:
- Enables definitive removal of the lesion.
- Provides tissue for histopathological analysis to confirm the diagnosis.
- Reduced recurrence if entire lesion excised.
- Simple, well-tolerated day-case procedure.
Disadvantages:
- Minor scar formation possible.
- Slightly longer healing time compared to destructive methods.
- Rare risk of infection, bleeding, or delayed wound healing.
Recurrence and Follow-up
- Warts can recur if small viral remnants remain in the tissue or if the immune system remains susceptible.
- Surgical removal reduces this risk compared to superficial treatments.
- Maintaining good skin hygiene, avoiding sharing personal items, and treating any underlying immunosuppression can minimise recurrence.
Post-Operative Care (After Excision)
- Keep the area clean and dry for the first 24 hours.
- After that, gentle cleaning with mild antiseptic solution once daily.
- Topical antibiotic ointment and a small dressing for 3–5 days.
- Avoid soaking, friction, or trauma to the area until healing is complete (usually 7–10 days).
Attend scheduled follow-up to review wound healing and histopathology results.
Possible Complications
- Minor bleeding or oozing
- Infection (rare; managed with antibiotics if required)
- Local scarring or pigmentation changes
- Recurrence, particularly in viral warts
- Discomfort for a few days after treatment
Why Choose MACS Clinic, Watford
- All procedures performed by qualified plastic surgeons under aseptic conditions.
- Facility for histopathological confirmation to ensure accurate diagnosis.
- Comprehensive aftercare and follow-up.
- Evidence-based management tailored to individual needs and skin type
Summary Table
| Treatment Type | Histopathology Possible | Recurrence Risk | Scarring Risk | Pain/Recovery |
| Chemical / Cryotherapy | No | Moderate | Low | Minimal |
| Laser / Coagulation | No | Moderate | Low-Moderate | Minimal |
| Surgical Excision | Yes |
Conclusion
While most warts are harmless, proper diagnosis is crucial — particularly in adults and immunocompromised patients.
At MACS Clinic, we prioritise surgical excision with histopathological confirmation to ensure that every lesion is accurately identified and safely treated.
This approach combines medical safety with aesthetic precision for optimal outcomes.


